Identifying the Factors Contributing to Treatment Abandonment in Childhood Cancers at a Tertiary Care Hospital in Pakistan
Abstract
Background: Despite advances in pediatric cancer treatment, survival rates in low- and middle-income countries (LMICs), such as Pakistan, remain low. Treatment abandonment, driven primarily by socioeconomic barriers and limited access to specialized care, is a leading cause of poor outcomes. This study aimed to identify factors associated with treatment abandonment among pediatric cancer patients.
Methodology: This prospective cohort study was conducted at the Pediatric Oncology Department, The Children’s Hospital, Pakistan Institute of Medical Sciences (PIMS), Islamabad, from January to December 2024. A total of 104 pediatric cancer patients aged < 14 years were included. Baseline interviews were conducted with parents to assess demographic and treatment-related factors at the time of diagnosis. Follow-up interviews were conducted to identify reasons for treatment abandonment, along with perceived challenges during treatment.
Results: Among 104 patients, 18 (17.3%) abandoned treatment, while 86 (82.7%) adhered to it. Common challenges included long travel distances (60.6%) and frequent hospital visits (82.7%). The leading reasons for abandonment were financial difficulties (61.1%) and geographical barriers (16.7%). Lower maternal education and the presence of treatment-related side effects were significantly associated with abandonment (p < 0.05). Male patients had higher compliance (61.6%) than females (38.4%). Patients diagnosed with solid tumors (38.9%) and leukemia (33.3%) indicated the highest abandonment rates. Most patients (63.4%) tolerated treatment well, and 66.3% perceived it as highly effective.
Conclusion: Treatment abandonment remains a major barrier to improved outcomes in pediatric oncology in Pakistan. Strengthening financial support, decentralizing services, and implementing patient-centered interventions are critical to improving adherence and survival in this setting.
Keywords: Treatment abandonment, pediatric cancer, financial barriers
Introduction
Pediatric cancer remains a major global public health concern, with approximately 400,000 new cases diagnosed annually in children and adolescents under the age of 191. Despite significant advances in diagnosis and treatment, the burden of childhood cancer is unequally distributed. While survival rates in high-income countries (HICs) exceed 80% due to early diagnosis, specialized care, and multidisciplinary support, outcomes in low- and middle-income countries (LMICs) remain substantially lower, often below 30%2,3. In Pakistan, for instance, survival rates for pediatric cancers are estimated to be as low as 20%, reflecting serious gaps in the availability, accessibility, and continuity of care4.
A critical yet preventable contributor to these poor outcomes is treatment abandonment, which refers to the failure to initiate or continue treatment for four or more consecutive weeks, excluding valid medical or administrative reasons5. This phenomenon is alarmingly common in LMICs, where structural healthcare barriers intersect with socioeconomic vulnerabilities. A retrospective study from Karachi reported that 22.2% of pediatric patients abandoned treatment, 11.2% never initiated therapy, and 11.0% discontinued prematurely6. Contributing factors included cancer type, distance from treatment center, maternal education, and the guardian’s occupation.
The underlying causes of treatment abandonment are multifaceted, involving financial hardship, lack of disease awareness, logistical challenges, social stigma, and caregiver fatigue. Direct costs of treatment and indirect expenses such as transportation, accommodation, and income loss often overwhelm families7,8. Simultaneously, non-financial barriers such as poor communication with healthcare providers, cultural beliefs, and social isolation further discourage treatment adherence9,10. Despite growing recognition of these challenges, non-financial contributors remain underexplored in local research, resulting in gaps in evidence-informed policy and practice.
Globally, the urgency to address abandonment has been emphasized by initiatives like the WHO Global Initiative for Childhood Cancer, which aims to achieve at least a 60% survival rate for children with cancer worldwide by 203011. This aligns with Sustainable Development Goals 3 and 4, which target the reduction of premature mortality from non-communicable diseases, including cancer. Addressing abandonment is thus essential not only for improving clinical outcomes but also for promoting health equity and achieving international commitments.
However, most existing studies in Pakistan have relied on retrospective record reviews and lack caregiver perspectives, thereby limiting their capacity to inform meaningful interventions. To bridge this gap, the present study employs a mixed-methods approach combining hospital record audits with structured interviews of caregivers. The aim is to comprehensively identify the factors contributing to treatment abandonment among pediatric cancer patients at a tertiary care hospital in Pakistan. By generating context-specific insights, this study seeks to inform practical, evidence-based strategies to reduce abandonment, improve treatment adherence, and ultimately enhance survival outcomes in pediatric oncology.
Methodology
We conducted a prospective observational cohort study at the Department of Pediatric Oncology, Children’s Hospital, Pakistan Institute of Medical Sciences (PIMS), Islamabad, spanning from January 1 to December 31, 2024. The study aimed to assess the incidence of and factors contributing to treatment abandonment in pediatric cancer patients. Children aged 0–13 years with a histopathological confirmed diagnosis of any type of malignancy and newly registered for treatment were included. Patients with relapsed disease, those referred for palliative care only, or those with incomplete records were excluded. Prior to enrollment, written informed consent was obtained from parents or legal guardians, and assent was sought from children aged 7 years and above, where appropriate.
Baseline data were collected through structured interviews with parents or primary caregivers within the first two weeks of diagnosis, using a pre-tested questionnaire developed in consultation with pediatric oncology experts. The questionnaire collected information on socio-demographic characteristics (age, sex, residence, parental education, household income, number of dependents, and distance to the hospital), clinical information (cancer type, treatment modality, presence of financial support or insurance), and contextual factors (cultural beliefs, perception of cancer, family support, and awareness about treatment options). All patients were followed prospectively for six months through routine clinic visits and telephonic follow-ups. If a patient missed a scheduled appointment, up to three follow-up phone calls were made at one-week intervals.
Treatment abandonment was defined according to the International Society of Pediatric Oncology (SIOP) guidelines as failure to initiate or continue curative treatment for a period of ≥ 4 consecutive weeks without a documented medical reason. If a patient returned after a delay of four weeks or more, they were still considered to have abandoned treatment for analysis purposes. For all identified cases of abandonment, follow-up interviews were conducted either in-person or via telephone to determine specific reasons for discontinuation. The reasons were categorized into thematic areas, including financial constraints, transport and access issues, fear of chemotherapy or its side effects, dissatisfaction with healthcare services, stigma, and preference for traditional or alternative medicine.
The study received ethical approval from the Ethical Review Board (ERB) of PIMS Islamabad (Approval No. F.1-1/2015/ERB/SZAMBU/1232) and all ethical guidelines were strictly followed to maintain confidentiality and protect the rights of participants.
Data analysis was conducted using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics such as frequencies, percentages, means, and standard deviations were used to summarize patient characteristics. Associations between socio-demographic and clinical variables and treatment abandonment were assessed using the Chi-square (χ²) test. A p-value < 0.05 is considered statistically significant.
Results
A total of 104 pediatric cancer patients were included in the study, of whom 18 (17.3%) abandoned treatment and 86 (82.7%) completed their prescribed care. The mean age of participants was 6.2 ± 3.3 years, and the majority were male (60.6%) and resided in rural areas (66.3%). Maternal education was low, with 66.3% of mothers having no formal education. The monthly household income was below 30,000 PKR in 73.1% of families, with a mean income of 23,846.15 PKR. Treatment support or funding was entirely self-supported by 49.0%, partially subsidized in 18.3%, and fully covered by government or charitable donors in 32.7% cases.
Leukemia was the most common diagnosis (42.3%), followed by lymphoma (23.1%), solid tumors (20.2%), brain tumors (6.7%), and others (7.7%). Treatment-related side effects were reported in 31.7% of patients. The duration of treatment varied, with 13.5% treated for less than one month, 60.6% for 1–6 months, and 25.9% for more than six months.
Comparison between treatment abandoners (n=18) and completers (n=86) showed no statistically significant differences in age, sex, residence, or treatment duration (p > 0.05). However, lower maternal education and the presence of treatment-related side effects were significantly associated with treatment abandonment (p < 0.05). Male patients were more likely to complete treatment (61.6%) compared to females (38.4%). Although not statistically significant, patients from lower-income households showed a trend toward higher rates of treatment abandonment. Among patients who abandoned treatment, solid tumors (38.9%) and leukemia (33.3%) were the most frequent diagnoses.
Qualitative interviews with caregivers of abandoners reinforced the quantitative findings, citing financial stress, long travel distances, and limited understanding of side effects as major barriers. Table 1 provides a detailed comparison of demographic and treatment characteristics between the two groups.
Table 1. Comparison of Demographic and Treatment Characteristics between Treatment Abandonment and Treatment Compliance Groups
*Values are statistically significant (p < 0.05).
We further explored caregiver perceptions regarding the treatment process. The treatment was well-tolerated by 63.4%, with 66.3% perceiving it as highly effective. However, logistical challenges were substantial, including 60.6% traveled more than 50 km to reach the hospital, and 82.7% required weekly visits. Public transportation was the primary mode (91.3%), and most families incurred travel costs between 1,000 and 2,500 PKR. Despite these challenges, 93.3% of caregivers reported clear or very clear communication with healthcare professionals. Table 2 summarizes perceived barriers in the treatment process.
Table 2. Perceived Barriers in the Treatment Process of Pediatric Cancer Patients (n = 104)
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Tolerance to treatment | ||
| Well-tolerated | 66 | 63.4 |
| Moderately tolerated | 27 | 26 |
| Poorly tolerated | 11 | 10.6 |
| Perceived effectiveness of treatment | ||
| Low | 14 | 13.5 |
| Moderate | 21 | 20.2 |
| High | 69 | 66.3 |
| Distance to treatment hospital | ||
| < 10 km | 9 | 8.7 |
| 10-20 km | 11 | 10.6 |
| 21-50 km | 21 | 20.2 |
| > 50 km | 63 | 60.6 |
| Frequency of visits required | ||
| Weekly | 86 | 82.7 |
| Bi-weekly | 13 | 12.5 |
| Monthly | 5 | 4.8 |
| Transportation modes | ||
| Public transportation | 95 | 91.3 |
| Private transportation | 7 | 6.7 |
| No transportation available | 2 | 1.9 |
| Travelling costs (in PKR) | ||
| < 1,000 | 11 | 10.6 |
| 1,000-2,500 | 47 | 45.2 |
| 2,501-50,000 | 33 | 31.7 |
| > 5,000 | 13 | 12.5 |
| Communication with healthcare professionals | ||
| Clear | 42 | 40.4 |
| Very clear | 55 | 52.9 |
| Sometimes unclear | 4 | 3.8 |
| Often unclear | 3 | 2.9 |
Among the 18 patients who abandoned treatment, the most commonly cited reason was financial difficulty (61.1%). Other reasons included geographical inaccessibility (16.7%), preference for alternative care facilities (11.1%), treatment-related toxicity (5.6%), and disease progression (5.6%). These findings are depicted in Figure 1, which categorizes reasons for abandonment as reported by caregivers.
Qualitative narratives further illustrated these challenges, including a caregiver who shared, “We sold our livestock twice, but traveling every week became impossible for us. We had to choose between feeding the rest of the children and continuing the treatment of our child.”
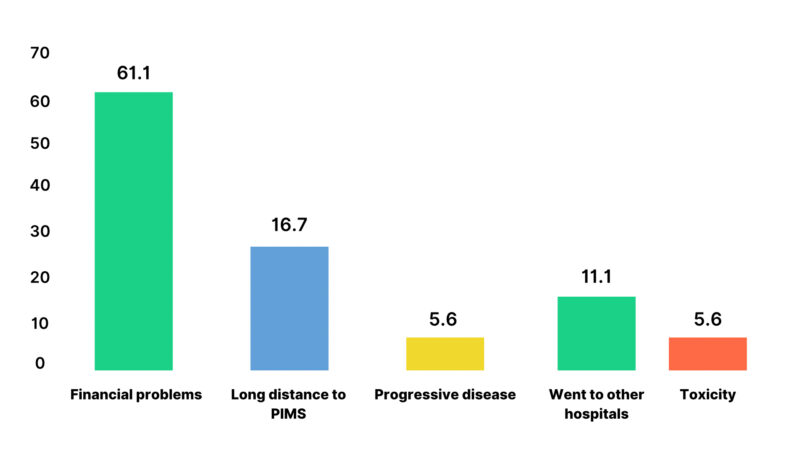
Figure 1. Reported Reasons for Treatment Abandonment
Discussion
Treatment abandonment remains a persistent barrier to improved pediatric oncology outcomes in LMICs, where survival rates continue to lag behind those in HICs. In this prospective cohort study conducted at a tertiary care hospital in Pakistan, we observed a treatment abandonment rate of 17.3%, which is significantly lower than the rates reported in other studies. For example, abandonment has been reported at 22.2% in Karachi6, 10-63% in India12, and 20.1% in Bangladesh13. This comparatively lower rate may reflect gradual improvements in healthcare access, targeted programmatic interventions, and community-level engagement to support treatment adherence. Nonetheless, the treatment abandonment rate remains significantly high compared to abandonment rates of less than 3% in HICs, where systems of universal health coverage and comprehensive psychosocial support substantially mitigate treatment discontinuation14. These findings emphasize the ongoing need for localized, evidence-informed strategies to further reduce abandonment in LMICs such as Pakistan.
Contrary to prior assumptions15,16,17,18, this study found no statistically significant association between treatment abandonment and demographic variables such as age, sex, place of residence, household income, financial assistance, or cancer type. However, two key predictors including low maternal education and the presence of treatment-related side effects were significantly associated with treatment abandonment. These results highlight the influence of social and experiential factors over demographic characteristics in determining adherence.
Maternal education emerged as an important determinant of treatment continuity. Among those who abandoned treatment, 72.2% had mothers with no formal education, compared to 61.6% in the compliant group. These findings align with studies from India and Iran, which highlight the role of maternal health literacy in facilitating understanding of treatment plans and navigating healthcare systems19,20. Conversely, studies from Ethiopia have shown that infrastructural and logistical barriers can sometimes outweigh the influence of parental education, indicating the context-dependent nature of this association21,22. Investing in caregiver-focused health education may therefore be a transformative strategy to reduce abandonment in low-resource settings like Pakistan.
While sex was not statistically associated with abandonment in this study, the observed trend of higher treatment compliance among male children reflects sociocultural norms in South Asia, where male health is often prioritized during financial hardship. Previous studies from India and Bangladesh have shown similar patterns12,13, though a systematic review by the George Institute reported inconsistent gender-based disparities across LMICs3. This underscores the need for gender-sensitive policies and proactive community engagement to ensure equitable access to pediatric oncology services.
Although 83.3% of those who abandoned treatment came from households earning < 30,000 PKR and 66.7% resided in rural areas, neither variable was a statistically significant predictor of abandonment. These findings are consistent with recent literature which suggests that socioeconomic and geographic variables exert greater influence when compounded by healthcare inaccessibility or weak caregiver support systems23,24. In contrast, in settings like Peru, where infrastructure and support are limited, rural residence has shown a stronger association with treatment dropout25. This indicates that strategic interventions such as transport subsidies, temporary lodging near hospitals, and caregiver support services may mitigate the impact of poverty and rurality on treatment adherence.
While a greater proportion of treatment completers received financial assistance (51.2%) compared to abandoners (38.9%), this difference was not statistically significant. Nevertheless, this trend may signal gaps in the scope, targeting, or adequacy of current financial aid programs. Evidence from Nepal and Latin America suggests that financial support is most effective when comprehensive covering direct and indirect costs and integrated with psychosocial and case management services26,27. In our context, partial or poorly structured financial support may fail to fully address treatment-related economic hardship.
Treatment-related side effects were significantly associated with abandonment, reported by 33.3% of abandoners versus 15.1% of completers. This supports findings from Malawi, where caregivers misinterpreted chemotherapy toxicities as treatment failure or worsening illness28. The lack of anticipatory guidance and symptom relief likely contributed to fear, confusion, and discontinuation of care. To address this, structured side-effect management protocols and early caregiver education should be integrated into treatment pathways.
Among abandoners, the most frequent diagnoses were solid tumors (38.9%) and leukemia (33.3%), though these differences were not statistically significant. This may reflect perceptions of poor prognosis or overwhelming treatment demands, particularly in cases involving visible tumors or complex regimens. Similar findings from Ethiopia suggest that delayed surgeries and emotional distress may influence caregiver decisions to discontinue care25. Diagnosis-specific counseling and transparent, empathetic communication about expected outcomes may help mitigate these perceptions.
The majority of both abandoners (77.8%) and completers (73.3%) had treatment durations of less than six months. This underscores the first few months as a critical window where abandonment is most likely. Consistent with findings from Mostert et al. (2015), early treatment phases often involve emotional, logistical, and financial overload for families29. Interventions such as patient navigation services, early psychosocial counseling, and consistent caregiver follow-up during this period are essential to prevent dropout.
The findings from this study provide a comprehensive view of caregiver perceptions regarding the pediatric cancer treatment process and highlight both strengths and challenges within the system. A majority of caregivers (63.4%) reported that the treatment was well-tolerated, which is consistent with similar studies from India and Pakistan showing good tolerance30,31. This suggests effective clinical management of side effects in the study setting. However, a significant proportion (10.6%) found treatment poorly tolerated, indicating a need for improved supportive care and individualized symptom management strategies, particularly during intensive chemotherapy phases. Furthermore, 66.3% of caregivers perceived the treatment to be highly effective, reflecting strong caregiver confidence in the healthcare team and visible clinical improvement in children. This finding aligns with studies from other LMICs where perceived effectiveness was closely linked to trust in the system and continuous progress updates32. Nonetheless, a small group (13.5%) perceived low treatment effectiveness, which requires further exploration to address potential miscommunication, unmet expectations, or adverse outcomes.
Despite these positive perceptions, significant logistical challenges were reported. More than half (60.6%) of families had to travel over 50 kilometers to reach the treatment center, a barrier that is consistently observed across LMICs, including Pakistan6, India12, and Bangladesh13. This distance not only adds financial stress but also risks treatment delays and abandonment. Additionally, the majority (82.7%) required weekly hospital visits, which, although clinically necessary, increase the burden on families, particularly those from distant areas. Studies have shown that such frequent visits contribute to emotional exhaustion and loss of livelihood for caregivers33. Public transportation was the primary mode of travel for 91.3% of families, underscoring a lack of private transport or hospital-supported conveyance options. Public transport in LMICs is often unreliable, and dependence on it can lead to missed appointments, especially for immunocompromised children. Regarding cost, 45.2% of caregivers reported weekly travel expenses between 1,000–2,500 PKR, with 12.5% spending more than 5,000 PKR weekly. These costs are substantial and align with existing literature from regional hospitals, which identifies transport and lodging as major contributors to treatment-related out-of-pocket expenses, often leading to financial hardship28.
Interestingly, despite these burdens, communication between caregivers and healthcare providers emerged as a strong point. A combined 93.3% of caregivers described the communication as either “clear” or “very clear,” a finding that is significantly better than those reported in other LMIC settings, where up to 30% of caregivers describe unclear communication. This suggests effective training and commitment to family-centered care at the facility, likely contributing to the high perception of treatment effectiveness and tolerance. Good communication is not only critical for building trust but also for ensuring adherence, improving psychological resilience, and empowering caregivers to participate in decision-making34,35. The positive perception in this domain should be institutionalized and scaled across other facilities through continuous training and caregiver feedback mechanisms.
The analysis of treatment abandonment among pediatric cancer patients revealed that financial difficulty was the most dominant reason, reported by 61.1% of caregivers. This finding aligns closely with multiple recent studies across LMICs, where financial burden consistently emerges as the primary driver of treatment abandonment. For instance, a study from India reported that 59.9% of pediatric cancer patients who abandoned treatment did so due to out-of-pocket expenses, including medication, transport, and accommodation costs36. Similarly, a study conducted in Egypt found that 64% of abandonment cases were associated with economic hardship, exacerbated by loss of caregiver income during treatment37. In Pakistan, Siddiqui et al. (2018) observed a 22.0% abandonment rate due to High cost of care and lack of supportive systems such as education, counseling, psychosocial support6. These findings emphasize that direct treatment costs are only one aspect of the financial strain; hidden and indirect expenses are equally devastating for low-income families.
The second most reported cause was geographical inaccessibility (16.7%), which is consistent with findings from the WHO Global Initiative for Childhood Cancer (2021), highlighting that long travel distances and poor transport infrastructure contribute to missed appointments and eventual dropout in LMICs38. A retrospective cohort study from Zambia (2008–2010) revealed that shorter distance to the pediatric oncology center was associated with lower odds of treatment abandonment, highlighting distance as an independent predictor of dropout 39. In Malawi, among children with lymphoma (2013–2016), travel time ≥ 4 hours was associated with nearly threefold higher risk of treatment abandonment28. In Pakistan, a study from Karachi’s Indus Children’s Cancer Hospital found that children from outside Karachi particularly from distant or rural areas were significantly more likely to abandon treatment, with travel-related challenges such as lack of transport and accommodation playing a key role6.
A smaller proportion (11.1%) cited preference for alternative care facilities, which could reflect dissatisfaction with hospital services, cultural beliefs, or reliance on traditional healers. This mirrors findings from Nigeria, where 13% of caregivers discontinued standard treatment in favor of spiritual or herbal remedies, often due to perceived lack of improvement or poor provider communication40. A similar trend was observed in India, where families abandoning formal treatment for spiritual or alternative healers, often driven by distress over treatment side effects or perceived poor healthcare provider communication 36. These patterns point to a need for better patient education, cultural sensitivity, and community engagement strategies to ensure families remain within the formal care system.
Treatment-related toxicity and disease progression were each responsible for 5.6% of abandonment cases. These findings are in line with a retrospective study from Kenya, where 7% of patients dropped out due to overwhelming side effects or belief that the disease was terminal41. Likewise, a Brazilian study reported that 6% of abandonment cases were associated with disease advancement, leading families to lose hope and discontinue therapy42. While these percentages may seem small, they represent a group of vulnerable families needing targeted psychosocial support, effective symptom management, and honest yet empathetic prognostic communication.
This study reinforces the multifactorial nature of treatment abandonment, with financial difficulty and geographical inaccessibility as the most pressing issues, followed by caregiver beliefs, treatment toxicity, and disease progression. These findings are broadly consistent with current regional and global literature, highlighting the structural inequities that continue to hinder treatment completion in LMICs. Healthcare systems must prioritize financial protection schemes, transport support, decentralization of services, and culturally responsive communication to improve retention in pediatric oncology programs. Without addressing these upstream barriers, clinical improvements alone will not be sufficient to close the survival gap in childhood cancers.
Conclusion
This study highlights treatment abandonment as a complex, multifactorial issue among pediatric cancer patients in low-resource settings such as Pakistan. Financial hardship was the most common reason, driven not only by medical costs but also by indirect expenses like transport, lodging, and lost income. Geographical inaccessibility further contributed, especially for rural families lacking transport support. Low maternal education and treatment-related toxicities were also significant predictors, underscoring the importance of caregiver health literacy and symptom management. Interestingly, factors such as sex, income level, and rural residence alone did not independently predict abandonment, suggesting systemic barriers play a larger role. Addressing this issue requires a holistic approach strengthening financial support, decentralizing services, improving caregiver education, and enhancing psychosocial and communication support to keep families engaged in care.
Competing Interests: The authors declare no competing financial interests.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
License
© Author(s) 2025.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, and unrestricted adaptation and reuse, including for commercial purposes, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
References
-
Ward ZJ, Yeh JM, Bhakta N, Frazier AL, Atun R. Estimating the total incidence of global childhood cancer: a simulation-based analysis. Lancet Oncol. 2019 Apr;20(4):483-93.
-
Howard SC, Zaidi A, Cao X, Weil O, Bey P, Patte C, et al. The My Child Matters programme: effect of public-private partnerships on paediatric cancer care in low-income and middle-income countries. Lancet Oncol. 2018;19(5):e252-e66.
-
Gupta S, Howard SC, Hunger SP, Antillon FG, Metzger ML, Israels T, et al. Treating childhood cancer in low- and middle-income countries. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, editors. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2015 Nov 1. Chapter 7.
-
Badar F, Mahmood S. Cancers among children and adolescents at a cancer hospital in Pakistan. J Ayub Med Coll Abbottabad. 2015;27(4):904-10.
-
Friedrich P, Lam CG, Kaur G, Itriago E, Ribeiro RC, Arora RS. Determining the incidence of abandonment of childhood cancer treatment in low-income and middle-income countries: a systematic review. Lancet Oncol. 2016;17(6):e291–e300.
-
Siddiqui DE, Ashraf MS, Iftikhar S, Belgaumi AF. Predictors of treatment abandonment for patients with pediatric cancer at Indus Children Cancer Hospital, Karachi, Pakistan. Pediatr Blood Cancer. 2018;65(2).
-
Mansell R, Purssell E. Treatment abandonment in children with cancer in Sub-Saharan Africa: Systematic literature review and meta-analysis. J Adv Nurs. 2018;74(4):800-8.
-
Bhakta N, Force LM, Allemani C, Atun R, Bray F, Coleman MP, et al. Childhood cancer burden: a review of global estimates. Lancet Oncol. 2019 Jan;20(1):e42-e53.
-
Susanah S, Modjaningrat IF, Sari NM, Suryawan N. Parental factors contribute to childhood cancer abandonment treatment during COVID-19. Glob Pediatr Health. 20226;9:2333794X221109767.
-
Henry M, Nichols S, Hwang JM, Nichols SD, Odiyo P, Watson M, et al. Barriers to communicating a cancer diagnosis to patients in a low- to middle-income context. J Psychosoc Oncol Res Pract. 2021;3(2):e049.
-
World Health Organization. Global initiative for childhood cancer. Available from: https://www.who.int/news/item/04-10-2018-global-initiative-for-childhood-cancer. Accessed 9 Jul 2025.
-
Arora B, Kanwar V. Childhood cancers in India: burden, barriers, and breakthroughs. Indian J Cancer. 2009;46(4):257-9.
-
Tahura S, Hussain M. Treatment refusal and abandonment in pediatric patients with acute lymphoblastic leukemia in Bangladesh. Int J Sci Res. 2017;6(8):643–5.
-
Howard SC, Metzger ML, Wilimas JA, Quintana Y, Pui CH, Robison LL, et al. Childhood cancer epidemiology in low-income countries. Cancer. 2008;112(3):461-72.
-
Sitaresmi MN, Mostert S, Schook RM, Sutaryo, Veerman AJ. Treatment refusal and abandonment in childhood acute lymphoblastic leukemia in Indonesia: an analysis of causes and consequences. Psychooncology. 2010;19(4):361-7.
-
Bonilla M, Rossell N, Salaverria C, Gupta S, Barr R, Sala A, et al. Prevalence and predictors of abandonment of therapy among children with cancer in El Salvador. Int J Cancer. 2009;125(9):2144-6.
-
Wang YR, Jin RM, Xu JW, Zhang ZQ. A report about treatment refusal and abandonment in children with acute lymphoblastic leukemia in China, 1997-2007. Leuk Res. 2011;35(12):1628-31.
-
Gupta S, Yeh S, Martiniuk A, Lam CG, Chen HY, Liu YL, et al. The magnitude and predictors of abandonment of therapy in paediatric acute leukaemia in middle-income countries: a systematic review and meta-analysis. Eur J Cancer. 2013;49(11):2555-64.
-
Arora RS, Eden TO, Kapoor G. Epidemiology of childhood cancer in India. Indian J Cancer. 2009;46(4):264-73.
-
Hazarika M, Mishra R, Saikia BJ, Bhuyan C, Nyuthe CW, Sarma A, et al. Causes of treatment abandonment of pediatric cancer patients – experience in a regional cancer centre in North East India. Asian Pac J Cancer Prev. 2019;20(4):1133-7.
-
Mirutse MK, Tolla MT, Memirie ST, Palm MT, Hailu D, Abdi KA, et al. The magnitude and perceived reasons for childhood cancer treatment abandonment in Ethiopia: from health care providers’ perspective. BMC Health Serv Res. 2022;22(1):1014.
-
Haileselassie W, Mulugeta T, Tigeneh W, Kaba M, Labisso WL. The situation of cancer treatment in Ethiopia: challenges and opportunities. J Cancer Prev. 2019;24(1):33-42.
-
Molla YM, Shad A, Wali R, Yimer MA. The magnitude and associated factors of childhood cancer treatment abandonment at the University of Gondar Comprehensive Specialized Hospital, Ethiopia. Sci Rep. 2025;15(1):10534.
-
Gull A, Ain RU, Faizan M, Riaz S, Mushtaq W, Iqbal L, et al. Caregiver-reported reasons and outcomes of treatment default among pediatric oncology patients at a tertiary care hospital in Pakistan: Pediatric cancer treatment default in Pakistan. Pak J Health Sci. 2025;6(6):37-41.
-
Vasquez L, Diaz R, Chavez S, Tarrillo F, Maza I, Hernandez E, et al. Factors associated with abandonment of therapy by children diagnosed with solid tumors in Peru. Pediatr Blood Cancer. 2018;65(6):e27007.
-
Khatiwoda SR, Dhungana RR, Sapkota VP, Singh S. Estimating the direct cost of cancer in Nepal: A cross-sectional study in a tertiary cancer hospital. Front Public Health. 2019 ;7:160.
-
Pérez-Cuevas R, Doubova SV, Zapata-Tarres M, Flores-Hernández S, Frazier L, Rodríguez-Galindo C, et al. Scaling up cancer care for children without medical insurance in developing countries: The case of Mexico. Pediatr Blood Cancer. 2013;60(2):196-203.
-
Stanley CC, van der Gronde T, Westmoreland KD, Salima A, Amuquandoh A, Itimu S, et al. Risk factors and reasons for treatment abandonment among children with lymphoma in Malawi. Support Care Cancer. 2018;26(3):967-73.
-
Amayiri N, Bouffet E. Treatment abandonment and refusal among children with central nervous system tumors in Jordan. Pediatr Blood Cancer. 2021;68(8):e29054.
-
Yadav SP, Rastogi N, Kharya G, Misra R, Ramzan M, Katewa S, et al. Barriers to cure for children with cancer in India and strategies to improve outcomes: a report by the Indian Pediatric Hematology Oncology Group. Pediatr Hematol Oncol. 2014;31(3):217-24.
-
Ahmad I, Ghafoor T, Ullah A, Naz S, Tahir M, Ahmed S, et al. Pediatric acute lymphoblastic leukemia: Clinical characteristics, treatment outcomes, and prognostic factors: 10 years’ experience from a low- and middle-income country. JCO Glob Oncol. 2023;9:e2200288.
-
Magrath I, Steliarova-Foucher E, Epelman S, Ribeiro RC, Harif M, Li CK, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013;14(3):e104-16.
-
Mensah ABB, Nunoo H, Mensah KB, Okyere J, Dzomeku VM, Apiribu F, et al. Impact of childhood and adolescence cancer on family caregivers: a qualitative analysis of strains, resources and coping behaviours. BMC Psychol. 2023;11(1):361.
-
Graetz DE, Garza M, Rodriguez-Galindo C, Mack JW. Pediatric cancer communication in low- and middle-income countries: a scoping review. Cancer. 2020;126(23):5030-9.
-
Chiragh S, Rehman A, Ahmad S. Financial toxicity of cancer treatment and its impact on quality of life in tertiary care public sector hospital. J Med Sci. 2017;25(3):313–8.
-
Alam A, Kumar A. Prevalence, predictors, causes of treatment refusal and abandonment in children with acute lymphoblastic leukaemia over 18 years in North India. Treatment phase affecting factors: A step towards better focussed counselling. Cancer Epidemiol. 2018;57:53-9.
-
Ghazawy ER, Mohammed ES, Mahfouz EM, Abdelrehim MG. Determinants of caregiver burden of persons with disabilities in a rural district in Egypt. BMC Public Health. 2020;20(1):1156.
-
Lima RAG, Lopes-Júnior LC, Maia EBS, Fuentes-Alabi S, Ponce MLV. Global Initiative for Childhood Cancer Control: Increasing access, improving quality, saving lives. Rev Lat Am Enfermagem. 2023;31:e3998.
-
Slone JS, Chunda-Liyoka C, Perez M, Mutalima N, Newton R, Chintu C, et al. Pediatric malignancies, treatment outcomes and abandonment of pediatric cancer treatment in Zambia. PLoS One. 2014;9(2):e89102.
-
Asuzu CC, Akin-Odanye EO, Asuzu MC, Holland J. A socio-cultural study of traditional healers’ role in African health care. Infect Agent Cancer. 20194:15.
-
Njuguna F, Mostert S, Slot A, Langat S, Skiles J, Sitaresmi MN, et al. Abandonment of childhood cancer treatment in Western Kenya. Arch Dis Child. 201499(7):609-14.
-
Ferman S, Lima FFDS, Lage CRS, da Hora SS, Vianna DT, Thuler LC. Preventing treatment abandonment for children with solid tumors: A single-center experience in Brazil. Pediatr Blood Cancer. 2019;66(7):e27724.





