Economic Pressures and the Unspotted Impact of Inflation on Mental Health and Burnout among the Pharmacists Working in Urban Egyptian Hospitals
Abstract
Background: Rising inflation and the sharp decline of the Egyptian pound since 2020 have intensified financial pressures on healthcare workers, including pharmacists. This study examines how inflation‑related financial stress affects mental health and burnout among pharmacists working in urban governmental hospitals in Egypt.
Methodology: A descriptive cross-sectional survey was conducted among pharmacists in metropolitan public hospitals. Data were collected using a structured online questionnaire developed by the research team and refined through expert review and pilot testing. The survey assessed socio-demographic characteristics, perceived financial situation, mental health status, burnout indicators, and coping strategies. Burnout was measured through a direct self-reported item regarding consideration of leaving one’s job due to burnout, while financial status was rated on a 5‑point scale. Descriptive statistics were used to summarize key variables.
Results: A total of 111 pharmacists participated. Financial strain was common, with 20.7% rating their financial situation as poor and 50.5% as fair. Mental health varied: 56.8% reported good or very good well-being, while 14.4% reported poor mental health. Burnout was substantial, as 62.2% havd considered leaving their job due to burnout, and 69.4% reported that financial stress influenced their career decisions. Workplace support was limited, with 34.2% reporting poor or very poor support and 77.5% noting a lack of resources to manage stress. Coping strategies included reallocating expenses (37.8%) and taking on additional work (11.7%), yet only 29.7% sought professional help.
Conclusion: Inflation and economic insecurity are strongly associated with financial stress, mental health challenges, and burnout among hospital pharmacists in Egypt. Targeted policies that reduce financial burdens, strengthen workplace support, and expand mental health resources are urgently needed to protect the well-being of healthcare professionals.
Keywords: Inflation, Burnout, Financial stress, Pharmacists, Mental Health.
Introduction
Health is defined as a complete state of physical, mental, and social well-being rather than just the absence of illness or disability, a principle established in the World Health Organization’s (WHO) 1948 Constitution. From this viewpoint, an individual’s financial and economic situation has a strong correlation with both their physical and mental health1.
Burnout among healthcare professionals, as defined by Christina Maslach, is a psychological syndrome resulting from prolonged occupational stress2. It is characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment, symptoms that reflect the emotional strain of demanding clinical roles. Burnout is widely recognized as a form of work-related mental health deterioration often emerging from chronic stress exposure3. Globally, it poses a significant challenge in the healthcare sector, driven by overwhelming workloads, emotional demands, systemic inefficiencies, and financial pressures. The latter, particularly in the context of rising inflation, has been identified as a key factor that exacerbates burnout among pharmacists, particularly under the umbrella of inflation4.
In early 2016, Egypt floated the pound against the dollar. The value of the Egyptian pound subsequently declined from EGP 8.8 to almost EGP 50 per U.S. dollar, representing a devaluation of around 470%. This dramatic decrease significantly reduced purchasing power due to rampant inflation and rising consumer prices, as illustrated in Figure 15.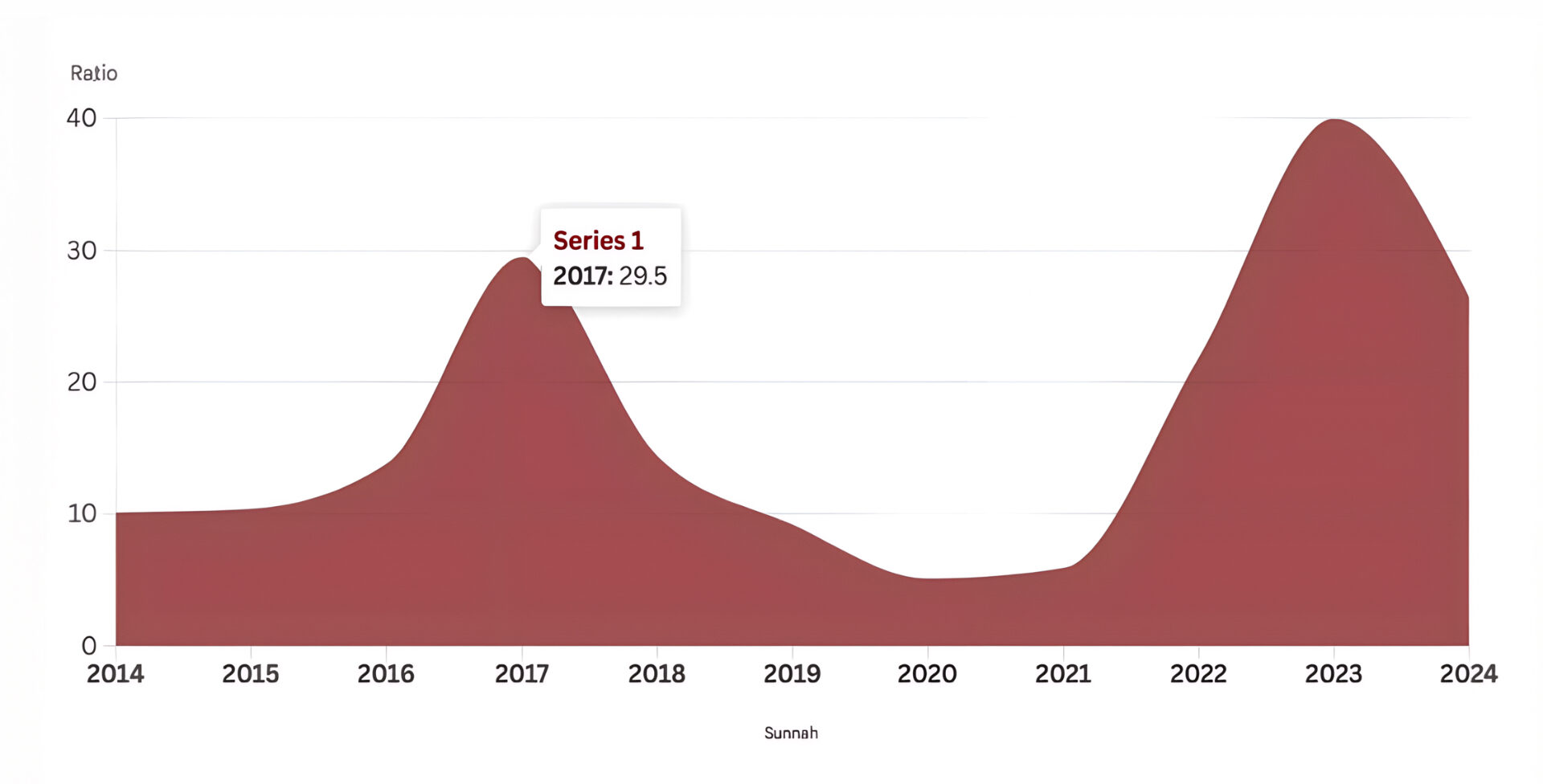
Figure 1: The inflation rates in Egypt in recent years (2014 – 2024)
Source: Central Agency for Public and Mobilization Statistics
A report from the Central Agency for Public Mobilization and Statistics (CAPMAS) indicates that in 2024, there were 1,114 pharmacists employed at educational hospitals and institutes within the governmental sector. In relation to the rising inflation rates, CAPMAS reports show that state public expenditure on health, as per the public budget for the years (2022/2023) and (2023/2024), stands at percentages of 6.2% and 4.9%, respectively, as illustrated in Figures 2 and 36,7.
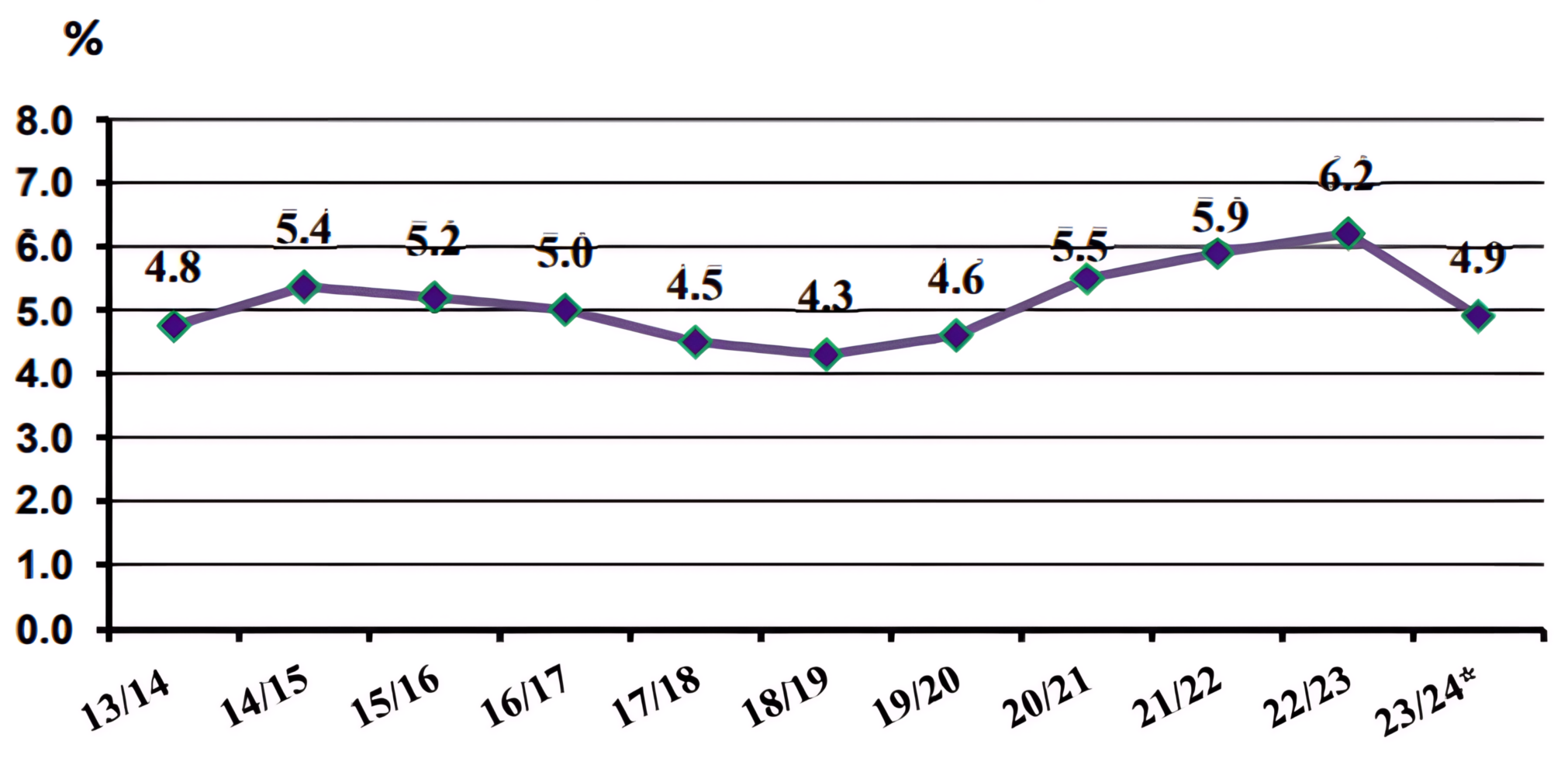
Figure 2: The percentages of expenditure on health to public expenditure of the state (2013/2014 – 2023/2024)
Source: Central Agency for Public and Mobilization Statistics
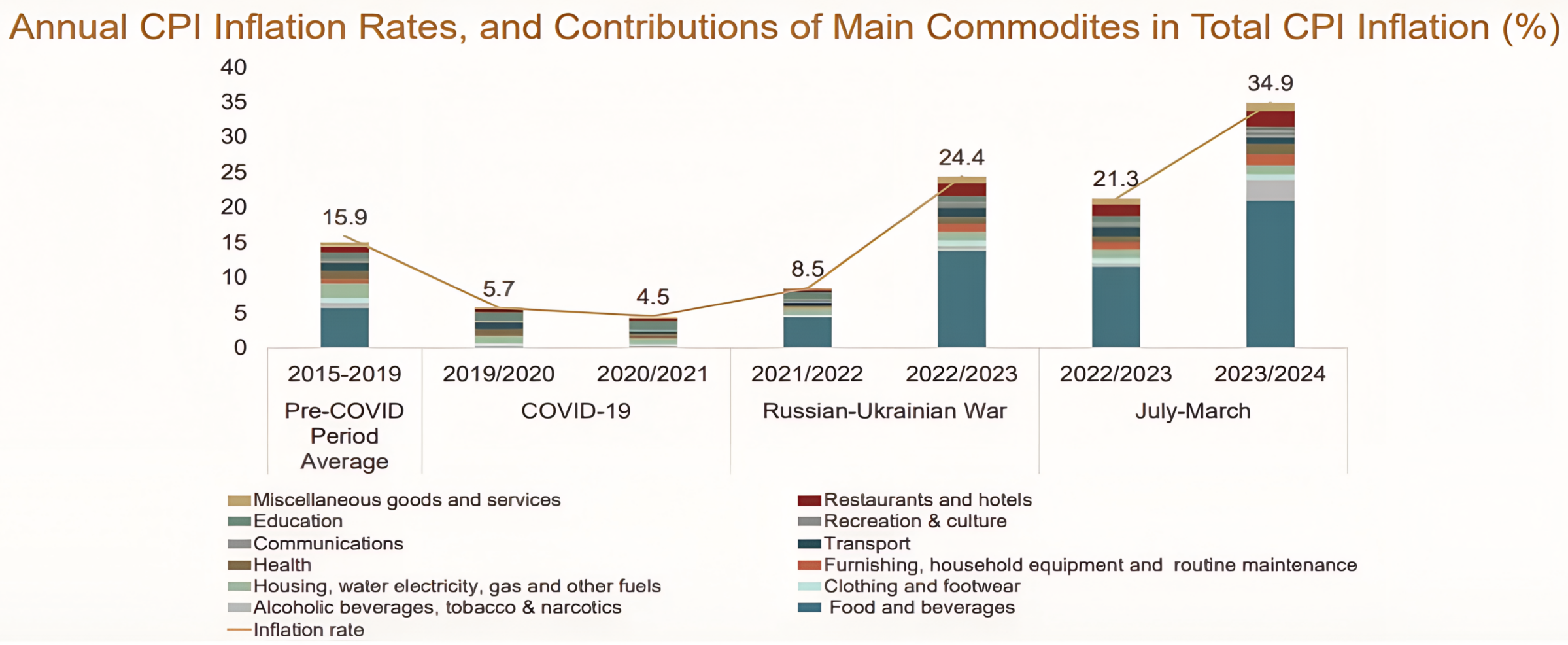
Figure 3: Annual consumer price index (CPI) inflation rates and contributions of main commodities, e.g., goods and services, in total CPI inflation percentage in the time period before COVID-19, going through the Russian-Ukrainian War, reaching to nowadays, and the recent elevation in inflation rates.
Source: Central Bank of Egypt
The reduction in the percentage of health expenditures from 2022/2023 to 2023/2024, as illustrated in Figure 2, diminishes the effective income of pharmacists employed in these hospitals and impacts the availability of essential medications, medical supplies, and updated equipment. This, in turn, affects the overall quality of patient care and treatment outcomes. Furthermore, restricted budgets intensify workplace issues, such as staff downsizing, which increases workloads on healthcare professionals6,7. This results in an occupationally stressful atmosphere, which is a significant contributor to burnout rates and mental health among employees.
In recent years, the contribution of pharmacists in hospitals, particularly in public ones, has notably improved patient safety and reduced administrative errors and medication-related issues8. However, this vital role is increasingly challenged by a growing global crisis of healthcare professional burnout, a severe and often under-recognized threat to healthcare systems worldwide, especially prevalent in Low and Middle-Income Countries (LMICs) where resource scarcity and systemic pressures are acute9.
Burnout in healthcare environments is extensively researched, with studies examining factors such as excessive workloads, emotional pressure, and systemic obstacles, including lack of resources, policy barriers, and administrative inefficiencies. It has seldom been explored how inflation specifically exacerbates these issues, especially in resource-constrained settings, as well as the lack of research into the relationship between inflation and burnout among hospital pharmacists. Moreover, the demanding nature of the healthcare profession necessitates urgent, focused research into this overlooked area.
Our research aimed to examine how inflation and financial strain affect burnout levels and mental health among pharmacists working in urban governmental hospitals in Egypt, following the significant rise in inflation rates from 2022 to 2024. This specific focus was chosen due to several factors inherent to the Egyptian context: governmental hospitals serve a vast segment of the urban population and operate within a centralized budgetary framework, making them particularly vulnerable to national economic pressures and policy shifts. Additionally, urban centers concentrate a significant proportion of the country’s healthcare workforce. While these findings offer crucial insights into this specific, large segment of pharmacists, it is important to consider these contextual factors when generalizing the results to pharmacists in rural areas, the private sector, or other healthcare systems. Ultimately, this study sought to dive deeper than basic observations of burnout rates by rigorously identifying the additional and distinct influence of economic instability and limited resources on pharmacists’ personal mental health, motivation, and overall professional performance in a critical sector.
Literature Review
The healthcare professionals face significant life quality changes because Egypt experienced its highest inflation rates according to Reuters reports in November 202410. Inflation is defined as the continuous increase in consumer prices combined with reduced purchasing power. It affects both economic systems and social structures. The inflation and currency crises have pushed sixty percent of the population into poor or vulnerable status11. The escalating cost of living has increased financial strain, resulting in mental health issues such as anxiety, depression, and burnout12.
A research conducted by Louie et al. established itself as one of the initial investigations about inflation challenges in 2022 and their impact on mental health, since they discovered that more inflation-related challenges lead to higher distress levels, which match the burnout criteria13.
A recent systematic review examining burnout among healthcare professionals in Qatar reported prevalence rates ranging from 10% to 38%, with pooled estimates of 17% and 20% based on fixed- and random-effects models, respectively. Burnout levels varied across professional groups, with the highest prevalence observed among pharmacists (51%) and the lowest among nurses (10%). The review also highlighted variability in burnout dimensions—emotional exhaustion, depersonalization, and reduced personal accomplishment, with emotional exhaustion affecting up to 45.7% of participants. Contributing factors included younger age, limited experience, heavy workloads, and insufficient organizational support, while protective factors such as effective coping strategies and empowering leadership were associated with lower burnout levels. These findings underscore the complex, multifactorial nature of burnout and the pressing need for targeted interventions within Qatar’s healthcare system14.
Research conducted in the United States demonstrated that inflation creates substantial mental health issues, which primarily manifest as anxiety and depression15. The strong connection between economic conditions and mental health has led policymakers and budget analysts to use economic data to guide their decisions16. Financial concerns about changes in income and daily expenses have been recognized as major contributors to burnout among healthcare workers17.
The medical community identifies burnout as a major health issue that affects healthcare professionals18. The risk of burnout depends significantly on age, along with job type and experience level, and relationship status19. The identification of these elements remains essential for preventing burnout syndrome development. The medical professionals in Egypt face elevated stress levels, anxiety, and burnout symptoms. Research indicates that Egyptian healthcare workers experience fatigue at a rate of 88.7% which exceeds the rates of 46.4% in the United States and 73.7% in China20. The research demonstrates an immediate requirement for successful mental health intervention strategies to minimize economic stress effects on healthcare staff.
Methodology
This descriptive, exploratory, cross-sectional study aimed to figure out the impact of inflation-related financial stress on burnout among pharmacists working in Egyptian governmental hospitals in urban cities, after the recent significant increase in inflation rates starting from 2022 until 2024. The study is descriptive in its objective to characterize the prevalence of financial stress, burnout, and mental health issues among the target population, while also being exploratory as it investigates potential relationships and less-understood dynamics between these variables in a novel context.
Participants were informed about the purposes and aims of the survey, also the confidentiality of all data was guaranteed. The questionnaire included both open-ended and closed-ended questions to collect quantitative and qualitative data on pharmacists’ burnout rates. Questions covered their current financial situation, the frequency of financial worries, and whether they had to take on additional work to meet financial needs. The survey also assessed the effects of financial stress on mental health, whether participants sought professional help, and the impact on burnout, including considerations of leaving their job or changing careers. Also, there were questions for assessing the strategies they used to cope with financial stress, mental health, or burnout. Data were obtained in the form of responders’ characteristics such as age, gender, marital status, number of children for married ones, and years of experience as a pharmacist.
Data Collection Instrument
A structured online questionnaire, administered via Google Forms, was self-developed by the research team to collect relevant data. The questionnaire was designed based on an extensive review of existing literature concerning financial stress, burnout, and mental health among healthcare professionals, ensuring content relevance to the study’s objectives. To ensure the clarity, appropriateness, and academic rigor of the questions, the entire questionnaire was reviewed and revised by a professor of research methodology and an expert in medical sociology before its implementation. It comprised several sections:
- Socio-demographic information: (e.g., age, gender, years of experience, marital status).
- Perceived Financial Situation: Questions assessing respondents’ subjective experience of their financial stability and the perceived impact of inflation.
- Burnout Assessment: Items derived from common constructs of burnout literature, focusing on emotional exhaustion, depersonalization, and personal accomplishment.
- Mental Health Status: Questions designed to capture self-reported mental well-being and common indicators of distress.
Before its full deployment, the questionnaire also underwent pilot testing with a small group of [e.g., 5-10] pharmacists who were not part of the main study sample. This pilot phase aimed to ensure practical clarity of language, ease of understanding, and cultural appropriateness of the questions in a real-world setting. Feedback from the pilot participants was used to refine and improve the questionnaire, leading to minor adjustments in wording for optimal comprehension. While formal psychometric validation (e.g., construct validity, reliability analysis) was not conducted for this specific questionnaire, the iterative process of expert review and pilot testing significantly strengthened its content validity and ensured the questions were carefully formulated to reflect established concepts in burnout and mental health research.
Assessment of Burnout
To determine the prevalence of burnout levels within the study population, the questionnaire included a specific, direct, self-reported item: ‘Have you considered leaving your job due to burnout?’ Participants who responded affirmatively (‘Yes’) to this question were operationally defined as having ‘reached burnout levels’ for this study. The frequency of these affirmative responses directly yielded the percentage reported in the results (i.e., 62.16%, n=69). It is important to clarify that this measure reflects pharmacists’ self-perception of burnout severity to the extent that it influences their consideration of job departure.
Perceived Financial Situation
Participants’ perceived financial situation was assessed using a single, self-reported item. Respondents were asked to rate their current financial status on a 5-point scale ranging from 1 (Very Poor), 2 (Poor), 3 (Fair), 4 (Good), to 5 (Very Good). This subjective assessment aimed to capture the individual’s personal perception of their financial well-being in the current economic climate, acknowledging that perceived financial stress can differ from objective financial indicators.
Analysis
The collected data were analyzed using descriptive statistical methods to summarize and interpret the findings. Microsoft Excel was utilized as the primary tool for data management and analysis, allowing for efficient organization, calculation, and visualization of results. The outcomes were represented through frequencies and percentages to provide a clear overview of the distribution and prevalence of key variables within the study population.
Results
A total of 111 pharmacists from urban governmental hospitals participated in this cross-sectional study. The findings are presented across several key domains, beginning with participant characteristics and then detailing perceptions of financial situation, mental health, burnout, and factors related to workplace support and coping strategies.
Sociodemographic Characteristics
Table 1 summarizes participants’ sociodemographic characteristics. Most respondents were young adults, predominantly female, with a substantial proportion residing in Cairo, and nearly half were married. These patterns reflect the demographic composition of pharmacists working in urban governmental hospitals.
Table 1: Demographic Characteristics of Respondents (n=111)
| Characteristic | Frequency (n) | Percentage (%) | ||
|---|---|---|---|---|
| Age | ||||
| Under 25 years | 18 | 16.22 | ||
| 25 - 34 years | 72 | 64.86 | ||
| 35 - 44 years | 19 | 17.12 | ||
| 55 years or above | 2 | 1.8 | ||
| Gender | ||||
| Female | 75 | 67.57 | ||
| Male | 36 | 32.43 | ||
| Marital Status | ||||
| Single | 46 | 41.44 | ||
| Married | 53 | 47.75 | ||
| Engaged | 7 | 6.31 | ||
| Divorced | 3 | 2.7 | ||
| Widowed | 2 | 1.8 | ||
| Years of Experience | ||||
| Less than 1 year | 12 | 10.81 | ||
| 1 - 5 years | 37 | 33.33 | ||
| 6 - 10 years | 33 | 29.73 | ||
| 11 - 15 years | 19 | 17.12 | ||
| More than 15 years | 10 | 9.01 | ||
| Current City of Residence | ||||
| Cairo | 74 | 66.67 | ||
| Giza | 36 | 32.43 | ||
| Alexandria | 1 | 0.9 | ||
| Financial Situation | ||||
| Very poor | 5 | 4.5 | ||
| Poor | 18 | 16.22 | ||
| Fair | 56 | 50.45 | ||
| Good | 29 | 26.13 | ||
| Very good | 3 | 2.7 | ||
Professional Experience
Regarding professional experience (detailed in Table 1), the distribution was as follows: 10.81% (n = 12) had less than one year of experience, 33.33% (n = 37) had 1-5 years, 29.73% (n = 33) had 6-10 years, 17.12% (n = 19) had 11-15 years, and 9.01% (n = 10) had more than 15 years of experience.
Perceived Financial Situation
Participants’ self-reported financial situations indicated significant concerns amidst the current economic climate. Table 1 illustrates the distribution of these perceptions. A combined 49.5% (n=55) of pharmacists rated their financial situation as ‘Poor’ or ‘Very Poor’ (Poor: 37.8%, n=42; Very Poor: 11.7%, n=13). Approximately 30.6% (n=34) described their financial status as ‘Fair’, while only 19.8% (n=22) reported it as ‘Good’ or ‘Very Good’ (Good: 18.9%, n=21; Very Good: 0.9%, n=1). These findings highlight a pervasive sense of financial strain within the study population.
Mental Health Status
Participants were asked to rate their overall mental health on a 5-point scale. The findings revealed a varied self-perception of mental well-being within the pharmacist cohort. A combined 56.8% (n=63) of pharmacists rated their mental health as ‘Good’ or ‘Very Good’ (Good: 41.4%, n=46; Very Good: 15.3%, n=17). Conversely, 14.4% (n=16) rated it as ‘Poor’ or ‘Very Poor’ (Poor: 11.7%, n=13; Very Poor: 2.7%, n=3). A substantial 28.8% (n=32) perceived their mental health as ‘Fair’. This self-reported assessment indicates that while a majority reported moderate to positive mental health, a notable proportion expressed concerns regarding their overall well-being.
Perceived Burnout and Job Retention
Consistent with our operational definition, a significant majority of participating pharmacists reported that burnout has a direct impact on their professional decisions. Specifically, 62.16% (n=69) of the pharmacists indicated that they had considered leaving their job due to burnout. This finding underscores a substantial proportion of the workforce experiencing burnout severe enough to impact their professional future and potentially contribute to workforce attrition. The professional choices of 69.37% (n = 77) participants were heavily affected by financial stress, which led them to decide whether to stay or leave their profession. This 69.37% (n=77) seems distinct from the 62.16% (n=69) related to burnout.
Workplace Support and Resources
Workplace support from superiors received ‘Fair’ ratings from 28.83% (n = 32) of respondents and ‘Good’ ratings from 24.32% (n = 27). Conversely, 23.42% (n = 26) reported ‘Poor’ support and 10.81% (n = 12) reported ‘Very Poor’ support, with 12.61% (n = 14) receiving ‘Very Good’ support. Furthermore, a substantial majority of respondents, 77.48% (n=86), indicated a lack of available workplace resources for managing stress and burnout.
Coping Strategies
The most popular coping strategies reported by pharmacists involved expense reallocation (37.84%, n = 42) and taking on extra work (11.71%, n = 13). The fact that nearly two-fifths of pharmacists resort to reallocating expenses highlights the direct impact of financial strain on their daily lives.
Challenges and Professional Help Seeking
While the majority of participants reported facing challenges, only 29.73% (n = 33) chose to seek professional help with these issues.
Discussion
Economic Pressures
Financial stress is strongly associated with burnout and poorer mental health among Egyptian pharmacists, but causality cannot be inferred from this cross-sectional study. The research demonstrates an association between financial strain and higher reported burnout and worse mental well-being, rather than proving a direct causal pathway. The Egyptian pound has declined substantially throughout the last two years, which has forced people from the average socio-economic class to maintain their financial stability. Research from the past has established that healthcare employee burnout is linked to this specific observation12. Healthcare workers faced extra challenges because their financial instability made their already demanding work conditions worse. Staff members working in low-income countries face extreme stress from financial demands, along with heavy workloads and insufficient staff and facilities18.
Cultural and gendered employment patterns shape how economic pressures affect pharmacists’ experiences. The research population consists mainly of female pharmacists who show a cultural preference for government employment over higher-paying positions according to Egyptian social norms. The study results show that fair financial status was reported by 72% of female respondents (n = 54/75) while male respondents reported this at a rate of 69% (n = 25/36). The study results from Louie et al. disagree with the finding that inflation-related hardships primarily affect men, resulting in higher distress levels13. Because our sample is predominantly female and many respondents are married, economic shocks may operate through household-level pathways (for example, redistributed financial responsibilities or reduced household buffers), which can amplify stress for both genders in different ways. The inflationary pressures forced Egyptian men to abandon traditional gender norms because nearly half of the male participants were married. The increased financial responsibilities placed on women after this shift may affect how their families handle financial challenges. The main response to the marital status question revealed that (Married) stood at 47.75% (n = 53), which shows that married people experience more financial stress due to increased household costs and family maintenance responsibilities.
Inflation-related financial concerns are linked to intentions to leave the profession and to higher reported fatigue and anxiety, with important workforce implications. Association between inflation-induced economic pressures and professional challenges among pharmacists was analysed, reporting 69.37% (n = 77) of respondent pharmacists commented on ‘How inflation influenced your decision to stay in or leave the pharmacy profession’ with ‘Strong influence’, among all participants, 62.16% (n = 69) were thinking of leaving their job. These findings suggest that economic pressures may contribute to turnover intentions, which can worsen staffing shortages and increase workload for remaining staff, creating a feedback loop that sustains burnout. This highlighted dissatisfaction, paired with an increase in unemployment and downsizing, has created a toxic environment that has taken a direct toll on the mental well-being of pharmacists. Such issues stand out when we compare them with international studies; the healthcare employees in Egypt face these challenges relatively more, with a fatigue rate of 88.7%, in comparison with the U.S and China, which were 46.4% and 73.7%, respectively20. The gap in reported fatigue suggests system-level differences in resourcing and social protection that may make pharmacists in Egypt more vulnerable to the combined effects of economic instability and workplace strain. This discrepancy indicates the unique strain Egyptian pharmacists face, possibly due to a combination of financial insecurity, understaffed departments, and overwork. Burnout flourishes in such an environment, which further exacerbates mental health issues.
More serious self-reported financial problems corresponded with increased anxiety and burnout symptoms among respondents, suggesting that mid-career pharmacists are particularly vulnerable. Among participants experiencing higher financial stress, 38.72% (n = 43) and 18% (n = 20) reported feeling constantly stressed, mainly due to burnout, particularly emotional exhaustion and depersonalization.
The concentration of respondents in the 1–5 and 6–10 years’ experience categories suggests that mid-career professionals, who often face growing household responsibilities and rising expectations at work, may lack sufficient coping resources and organizational support, increasing vulnerability to burnout. The survey results show that mid-career professionals face high vulnerability because most respondents fall into the 1-5 years and 6-10 years’ experience categories.
Recent evidence from low- and middle-income countries (LMICs) highlights that economic and institutional stressors significantly contribute to burnout and psychological distress among healthcare professionals. Systematic reviews have documented that frontline providers across LMICs frequently report high levels of emotional exhaustion, depersonalization, and reduced personal accomplishment21. For instance, a meta-analysis of primary health-care workers in LMICs found a pooled prevalence of 28.1% for high emotional exhaustion and 16.4% for high depersonalization22. In addition, during the COVID-19 pandemic, LMIC health workers faced exacerbated psychological burdens, including burnout, anxiety, and depression, due to infrastructural deficits, financial insecurity, and high work demands23.
Supervisor support and organizational resources are reported as inadequate by many respondents and likely moderate the relationship between financial stress and burnout. Most respondents rated their superior support as fair to good, but this shows there is still a need for better guidance and resources to manage stress effectively, since burnout rates are high. Limited quality or frequency of supervisory support and inadequate workplace resources (reported by 77.48% of respondents) may reduce employees’ ability to cope with external financial stressors, increasing the risk of sustained burnout. The quality and frequency of supervisor support need improvement to reduce some of the negative effects of burnout. Many respondents (77.48%) believe their workplace lacks sufficient resources to handle stress and burnout, which demonstrates the need for organizational changes to address these issues.
Low uptake of professional mental health services highlights barriers to help-seeking that organizations should address. The high stress levels reported by 40% of respondents, along with the constant stress experienced by many participants, show the necessity for financial and emotional assistance. Only 29.73% seeking professional help suggests stigma, limited access, time constraints, cost, or insufficient workplace mental health services, barriers that must be investigated and addressed to improve staff well-being. The low percentage of 29.73% of respondents who sought professional help raises concerns because it suggests barriers exist that prevent people from obtaining necessary mental health support.
Coping Strategies
Coping strategies reported by pharmacists are pragmatic but may not mitigate the psychological dimensions of burnout without organizational interventions. The data indicate that organizations need to develop active strategies that promote help-seeking behaviours while providing accessible mental health services at work. Managing strategies were also discussed with participating pharmacists, showing that a variety of mechanisms were aimed to cope with the influence of inflation and to face burnout syndrome, like revising their needs and reallocating expenses accordingly, and searching for additional jobs to raise their income were 37.84% and 11.71%, respectively. Individual financial coping (budgeting, moonlighting) addresses immediate economic needs but does not reduce workplace contributors to burnout (workload, staffing, support), so combined individual and organizational interventions are likely necessary. These strategies, while practical, suggest that coping mechanisms that primarily focus on financial solutions may not be sufficient to address the deeper mental health issues facing these professionals. Aligning with other studies, it is supposed that coping strategies could be beneficial as a prophylactic mechanism of psychological exhaustion, particularly in stressful conditions like the healthcare field19. Additionally, it should be noted that the mental health status of healthcare professionals, particularly pharmacists, could affect patients directly, whether in the form of diminished healthcare effectiveness and so reduced quality.
Policy Implications
Policy actions should target both financial protections and workplace improvements to protect pharmacists’ mental health and patient safety. In the last decades, pharmacists have been a crucial part of the healthcare team in hospitals as clinical pharmacy’s existence was becoming more significant in diminishing and limiting medication errors, having a positive impact on patient safety8. Policymakers should consider measures such as targeted funding to public hospitals, wage adjustments or social protections that offset inflationary losses, expanded workplace mental health services, and investments in staffing and supervisory training to reduce burnout and preserve clinical pharmacy functions. Based on this, policymakers need to establish regulations and measures that support workers’ mental well-being, especially under the umbrella of inflation, providing increased funding for public hospitals to enhance the working environment and lessen the burden, offering appropriate services that promote mental wellness, in addition to targeted counselling within the organizations, aiming to achieve a healthy workplace culture.
Study limitations restrict generalizability and preclude causal claims; future research should use longitudinal and broader sampling designs. Although this study offered useful information, it has a few limitations. First, there was a problem with generalization as the study sampled urban hospitals only, in addition to a small sample size, which may limit the relevance of the findings to rural areas and pharmacists working in other sectors. The self-administered online survey design introduces potential self-report and selection biases, and the cross-sectional nature of the data prevents establishing temporal or causal relationships between inflation, financial stress, and burnout. Also, self-administered and self-assessment online surveys may lead to self-report bias. Finally, cross-sectional analysis prevents making causal statements by comparing the same individuals in different circumstances; before and after 2022, that’s why longitudinal studies are better placed to provide explanations of causal relations, and here arises the deep need for future research.
Recommended next steps include a detailed literature synthesis and targeted workplace interventions to test whether reducing financial strain or improving organizational support lowers burnout. Future work should incorporate a thorough literature review that evaluates international and regional evidence on economic shocks and healthcare worker burnout, use longitudinal methods to clarify causal pathways, and pilot combined financial and organizational interventions to assess impact on turnover intentions, burnout scores, and patient-facing outcomes.
Conclusion
This study showed the impact of economic pressures and inflation on mental health and burnout levels of pharmacists working in urban Egyptian hospitals. The research reveals major difficulties affecting this workforce, which highlights the requirement for specific solutions to address healthcare professionals’ economic strain from inflation.
The survey results revealed that pharmacists experience major financial difficulties while dealing with mental health issues and burnout. The research demonstrated the immediate requirement for policies that would decrease financial burdens and enhance workplace environments, and provide mental health assistance to healthcare staff in areas with economic difficulties through institutional mental health support, such as counseling programs or resilience workshops. Future longitudinal studies may be performed on a larger sample of healthcare professionals for broader assessment, trying to find out other factors affecting mental health among this population.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
License
© The Author(s) 2025.
This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, and unrestricted adaptation and reuse, including for commercial purposes, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
References
-
Sieverding M, Hassan R. Associations between economic vulnerability and health and well-being in Egypt [Internet]. 2019 cited 2025 Jan 12; Available from: https://erf.org.eg/
-
Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016 Jun;15(2):103-11.
-
McCormack HM, MacIntyre TE, O’Shea D, et al. The prevalence and cause(s) of burnout among applied psychologists: a systematic review. Front Psychol. 2018 Oct 16;9:1897.
-
De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. 2020 Oct 28;13:171-83.
-
Mai Ali. Egypt’s economic divide: a threat to social stability. Zawia3 [Internet]. 2024 Dec 11 [cited 2025 Jan 12]; Available from: https://zawia3.com/en/lifting-subsidies/
-
CAPMAS. Health sector [Internet]. 2024 Mar [cited 2025 Jan 12]. Available from: https://www.capmas.gov.eg/Pages/StaticPages.aspx?page_id=5035
-
CBE. Financial stability report [Internet]. 2024 Mar [cited 2025 Jan 12]. Available from: https://www.cbe.org.eg
-
Sabry N, Abbassi M. Impact of a clinical pharmacist in the general hospital: an Egyptian trial. Pharmacology & Pharmacy. 2014;5:577-87.
-
Bitton A, Fifield J, Ratcliffe H, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. 2019 Aug 16;4(Suppl 8):e001551.
-
Reuters. Egypt’s inflation dips to near two-year low of 25.5% in November [Internet]. 2024 Dec 10 [cited 2025 Jan 12]. Available from: https://www.reuters.com/world/africa/egypts-annual-urban-consumer-price-inflation-255-november-2024-12-10/
-
Financial Times. Egypt’s economic woe spreads across all classes [Internet]. 2023 Feb 15 [cited 2025 Jan 12]. Available from: https://www.ft.com/content/13286c00-e0ca-46d7-92d5-83319372cbde
-
El Dabbah NA, Elhadi YAM. Burnout among frontline health professionals in two African countries: a cross-sectional study from Egypt and Sudan [Internet]. 2021 Sep 30. Available from: https://doi.org/10.21203/rs.3.rs-951355/v1
-
Louie P, Wu C, Shahidi FV, et al. Inflation hardship, gender, and mental health. SSM Popul Health. 2023 Jun 12;23:101452.
-
Albazoon F, Khogali F, Burjaq R, et al. Burnout among healthcare professionals in Qatar: a systematic review. Asian J Psychiatr. 2023 Jul;85:103601.
-
Pathak M, Mitra S, Pinnamraju J, et al. Stress due to inflation and its association with anxiety and depression among working-age adults in the United States. Int J Environ Res Public Health. 2024 Dec 29;22(1):26.
-
Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry. 2020 Feb;19(1):3-14.
-
Nowrouzi-Kia B, Sithamparanathan G, Nadesar N, et al. Factors associated with work performance and mental health of healthcare workers during pandemics: a systematic review and meta-analysis. J Public Health (Oxf). 2022 Dec 1;44(4):731-9.
-
El-Sayed EM, Mohamed AA, Saad DM. Work stress and burnout among healthcare workers in Egypt: a cross-sectional study. Egypt J Psychiatry. 2023;44(3):215-24.
-
Maresca G, Corallo F, Catanese G, et al. Coping strategies of healthcare professionals with burnout syndrome: a systematic review. Medicina (Kaunas). 2022 Feb 21;58(2):327.
-
Abdalgeleel SA, Moneer MM, Refaee AS, et al. Depression and fatigue among Egyptian health care workers: cross-sectional survey. J Public Health (Berl.). 2024;32:2153-62.
-
Dugani S, Afari H, Hirschhorn LR, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: a systematic review. Gates Open Res. 2018 Jun 11;2:4.
-
Wright T, Mughal F, Babatunde OO, et al. Burnout among primary health-care professionals in low- and middle-income countries: systematic review and meta-analysis. Bull World Health Organ. 2022 Jun 1;100(6):385-401A.
-
Deng D, Naslund JA. Psychological impact of COVID-19 pandemic on frontline health workers in low- and middle-income countries. Harv Public Health Rev (Camb). 2020 Fall;28





