Leukemia Cutis as the Initial Presentation of an Early Relapsed Acute T-Cell Lymphoblastic Leukemia: A Rare Paediatric Case Report
Abstract
Introduction: Acute leukemias account for up to 25-30% of childhood malignancies, with relapse occurring in 15-20% of the children. Skin lesions as the presenting manifestation of early combined relapse in T-ALL is extremely rare in children with no case reported till date. The mechanism of skin relapse is not yet fully known. We report an unusual case in which a 6-year-old male child presented with leukemia cutis (LC) as the initial symptom of early combined relapse in T-cell acute lymphoblastic leukemia (T-ALL).
Case Report: A six-year-old male patient presented with a painless nodular swelling with hyperpigmentation over the right upper part of chest after defaulting for four months after the completion of the induction of the ALL-IC-BFM-90 chemotherapy protocol administered due to the diagnosis of T-ALL. Molecular studies were negative for BCR-BL fusion and MLL-rearrangement. Minimal residual disease was <0.01% in the post-induction flow cytometry. Physical examination revealed a hard, painless, hyperemic, nodular lesion measuring 2×1 centimeter on the right upper part of chest (Figure 1).
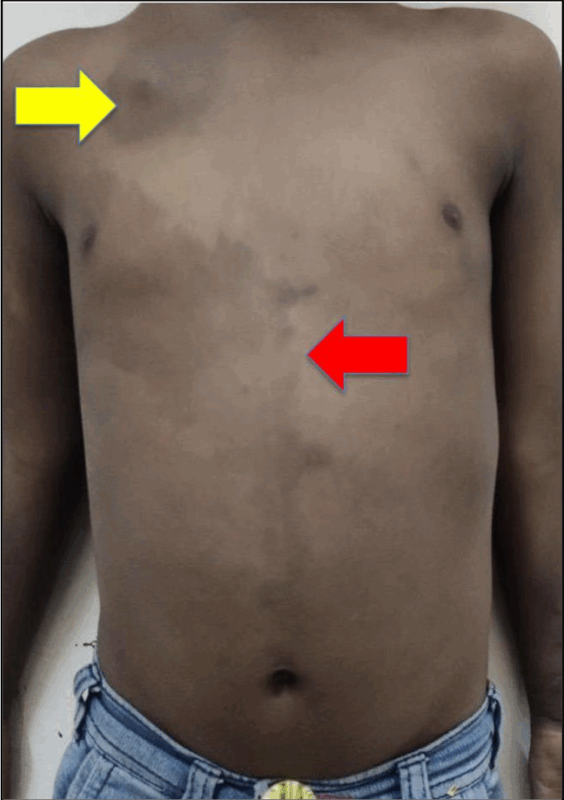
Figure 1: Image depicting café-au-lait macule (red arrow) and LC (yellow arrow) on the right upper part of chest
General examination revealed pallor, significant generalized lymphadenopathy, right preaxial polydactyly in the form of split thumb (Figure 2), multiple cafe-au-lait macules largest of size 16-centimeter over the right mammary area extending to midline (Figure 1). Anthropometry revealed proportionate short stature and per abdomen examination showed hepatosplenomegaly. Testis was normal in size.

Figure 2: Photographs of right and left hand showing right preaxial polydactyly in the form of split thumb
Atypical monomorphic infiltrates with the prominent nucleolus, narrow cytoplasm, and immunohistochemically stained with CD3, CyCD3, CD4, CD5, CD7 and CD8 were observed in the histopathological examination of the skin lesion (Figure 3). There was 69% blast in the bone marrow aspiration smear and cerebrospinal fluid was free of leukemic infiltrates. In view of suspected Fanconi anemia in the child Mitomycin-C chromosomal breakage analysis was done which was negative. The patient was started on UK-ALLR3 relapse protocol for combined relapse and the child succumbed due to complications of severe myelotoxicity on week-4 of induction.
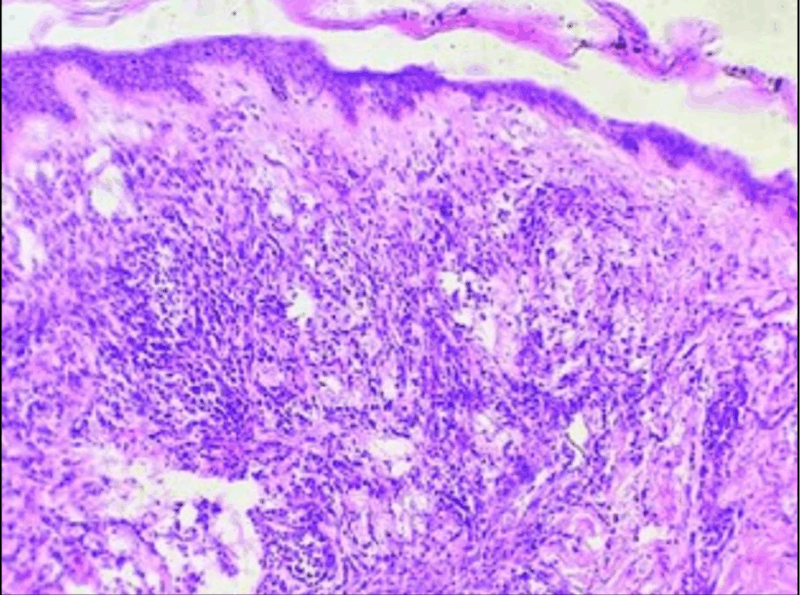
Figure 3: Biopsy of the skin torso showing diffuse dermal infiltrates of atypical mononuclear cells with destruction of adnexal structures (×100, H and E)
Discussion: Adult cases of T-ALL with LC is reported, but this is the first paediatric case report of T-ALL with LC as the initial manifestation of an early combined relapse. A recent study from Taiwan indicated that the median survival time of patients with LC is 7.2-months which was less in our study.
Conclusion: To summarize, although unusual, LC can be the first indication of the presence of T-ALL relapse. When skin lesions appear as multiple purplish red nodules or infiltrated plaques without additional symptoms, clinicians should contemplate the possibility of LC. Timely identification of LC may allow for more speedy instigation of treatment and thus improved prognosis.