A Child With A Disfigurement: Can Fungal Infection Be The Cause?
Abstract
Introduction: An eight-year-old male with a history of recurrent infections since infancy. He presented with progressive fungating skin lesions diagnosed as invasive skin Candidiasis complicated by keratomycosis in an immunocompromised child. This case highlights the importance of meticulous microbiological and histopathological work-up and appropriate treatment of fungal infections with unusual clinical features.
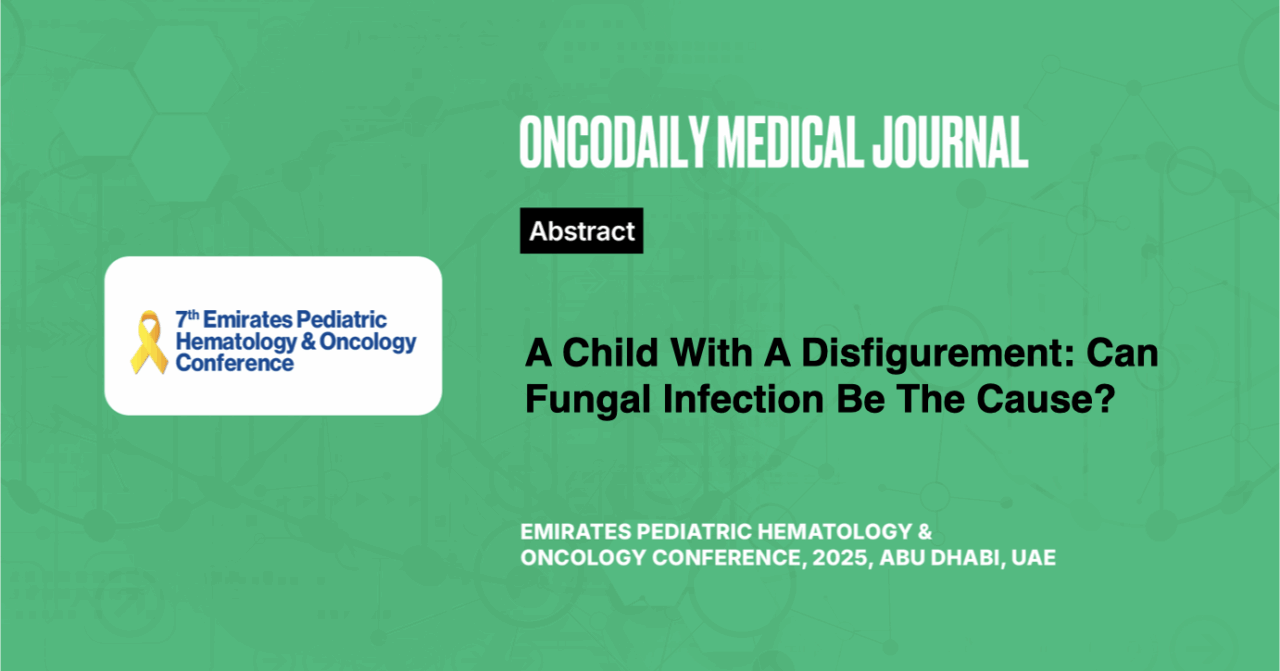
Case presentation: An eight-year-old African male child initially presented with a papillomatous lesion on the right eye, followed by a progressive fungating facial mass, multiple skin nodules, rashes all over the body, intermittent fever, and visual impairment. The child had a history of recurrent respiratory infections and skin rashes since infancy, diagnosed as chronic eczema along with exposure to pets and cattle, with no history of previous hospitalization or blood transfusion. There were no significant family histories of consanguinity or malignancy.

Figure 1: Fungating facial mass, and opacity in both eyes
Imaging, including CT scans and PET/CT, revealed multiple facial fungating masses and lymph node involvement. Histopathological examinations initially suggested atypical mycobacterial infection, but further investigation confirmed Candida Albicans as the causative organism.
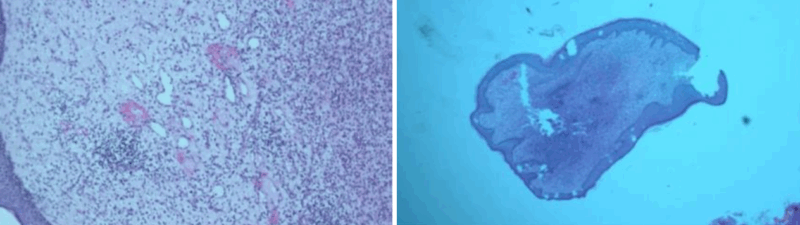
Figure 2: Atypical Mycobacterial Infection (AMI)
The patient received antifungal therapy, including voriconazole, but despite recurrent infections and persistent fever, the patient’s condition improved with the combined treatment of antifungals, antibiotics, and steroids. Immunological and genetic testing revealed a primary immune deficiency. Plans for hematopoietic stem cell transplantation are underway, along with cosmetic treatments to address the facial and visual impairments.
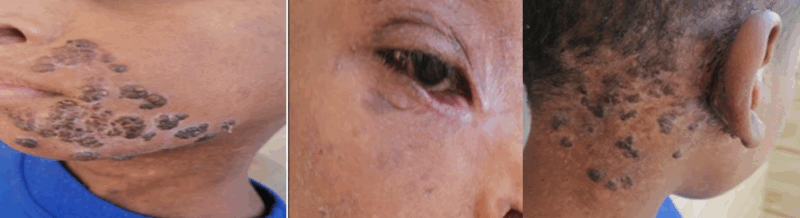
Figure 3: Response to antifungal treatment
In debilitated patients, invasive candidiasis is a common healthcare-associated infection, contributing significantly to morbidity, mortality, and high healthcare costs. Its diagnosis can be difficult and often delayed due to non-specific symptoms. The disease is typically diagnosed through culture from sterile sites, but sensitivity is only 50%. Neutrophils and mononuclear phagocytes play key roles in immune defense, triggering the production of protective cytokines.
Fungi can be part of ocular flora, with the risk of fungal keratitis varying based on geography, climate, and trauma. Fungal keratitis is hard to treat, and early diagnosis is critical. Accurate diagnostic materials are essential for treatment. For invasive candidiasis, early antifungal therapy, source control, and a combination of treatments (systemic, topical, and/or surgical) are essential for successful resolution.
Conclusion: Candidiasis is one of the most common causes of invasive fungal diseases in the immunocompromised. Key challenges to managing invasive candidiasis include prevention, early recognition, and rapid initiation of appropriate antifungal therapy.