Rare Case of Intracranial Recurrence of Osteosarcoma: Case Report and Review of Literature
Abstract
Introduction: Osteosarcoma is the most common malignant bone tumour in children. Though outcome has improved with multimodality treatment, up to one-third of patients develop recurrence. Metastatic disease is seen in 20% of patients with brain metastases being extremely rare in primary or recurrent setting.
Case presentation: 13-year-old male presented with pain, swelling over left paravertebral region with imaging showing a destructive lesion of single rib. Diagnosed as high-grade Osteosarcoma and initiated on chemotherapy, primary lesion progressed post 3 cycles. He underwent resection and had completed his treatment. Presented 2 months later with seizures, with CT head suggestive of metastatic recurrence. Patient was offered palliation and had succumbed three months later.
Conclusion: Brain metastases are unusual in osteosarcoma patients and they have a poor prognosis. This possibility should be kept when an osteosarcoma patient presents with neurological symptoms.
Introduction
Osteosarcoma is the most common malignant bone tumour affecting children, adolescents, and young adults1. More than 50% of cases arise in the long bones around the knee. Although survival for patients with high-grade osteosarcoma has improved with multi-agent chemotherapy and aggressive surgical control, up to one-third of patients experience recurrence, which remains challenging to treat. Approximately 15–20% of patients present with metastatic disease at diagnosis, most commonly involving the lungs and other bones. Brain metastases are exceedingly rare, either at initial presentation or during recurrence2. Outcomes for children with metastatic disease continue to be poor. Here, we report a rare case of osteosarcoma with both local and intracranial recurrence.
Case Report
A 13-year-old male presented with complaints of pain and swelling over the left paravertebral region of one month duration. CT Thorax revealed a destructive lesion of the left 7th rib with an associated soft tissue component of 11 x 6 cm. Biopsy from the lesion revealed a high-grade sarcoma with epithelioid and plump spindle cells in an osteoid matrix, suggestive of high-grade osteosarcoma (IHC: ERG-negative, Desmin-negative, SATB2-diffuse weak to moderate positive). CT thorax and bone scans revealed no lung or bone metastases.
He received neoadjuvant chemotherapy with Ifosfamide (3.6 g/m²), Adriamycin (60mg/m²), and Cisplatin (100mg/m²) (IAP), as per our institutional protocol. After three cycles of chemotherapy, response assessment with CT Thorax showed an interval increase in size of the primary lesion with moderate left-sided pleural effusion. He underwent excision of the tumour with resection of the 6th, 7th and 8th ribs and mesh repair of the defect. All four soft tissue margins (both lateral, superior and inferior) were positive for tumour. The histological response was poor, showing 70% viable osteosarcoma cells and only 30% necrosis. A second surgery was not considered because of the risk of morbidity. At the time of treatment, our institutional protocol for osteosarcoma was the IAP protocol, as it was not possible to administer high-dose methotrexate because of resource constraints. including the unavailability of methotrexate level monitoring and intensive supportive care. An alternate regimen was therefore not pursued, and the child received three additional cycles of IAP chemotherapy followed by surveillance.
Two months later, the child presented with three episodes of seizures of generalised tonic-clonic semiology. CT scan of the head revealed a 2-cm enhancing lesion in the right frontal region with perilesional oedema, most likely representing a metastatic focus (Figure 1). A meningioma was also considered in the differential diagnosis; however, the patient’s young age and the absence of any syndrome typically associated with pediatric meningiomas made this less likely. CT thorax revealed multiple soft tissue lesions at the surgical site, the largest 2.3x2cm and an intraspinal deposit at the T6-7 level, suggestive of local recurrence (Figure 2). There were no skeletal metastases on the bone scan.
Given the high clinical and radiological suspicion for metastases, the patient was diagnosed with a recurrence of osteosarcoma. After a discussion with the parents regarding the grave prognosis and limited chance of getting cured with further treatment, the focus of care was shifted to palliation. Consequently, a diagnostic brain biopsy was deemed unnecessary and was not performed. He was given palliative radiotherapy to the left chest wall and brain metastases at a dose of 20Gy in 5 fractions each. Three months later, the child presented with worsening of sensorium and succumbed to his illness.

Figure 1: Contrast-enhancing lesion (2 cm) with perilesional oedema noted in the right frontal region, with sclerosis of adjacent bone- metastasis appears likely
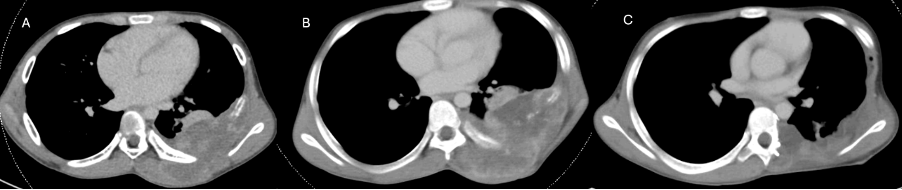
Figure 2: CT Thorax images at various time points. A-At presentation, B-Prior to surgery, C-At recurrence
Discussion
Most osteosarcoma recurrences (80%) present as pulmonary metastases, and other site recurrences are seen in only 2% cases3. The large size of the primary tumour and its axial location, as in our case, are established risk factors associated with the risk of recurrence in Osteosarcoma4. In addition, the poor histological response to chemotherapy and involved resection margins could have further heightened the risk5. While chemotherapy augmentation for poor histological response has not shown proven benefit6, the high-risk profile of this case may have justified consideration of an alternative methotrexate-based regimen. The median time to recurrence in relapsed osteosarcoma is approximately 1.6 years3. Patients with relapsed osteosarcoma are more likely to survive after the first relapse if they are < 18 years, had localized disease at diagnosis, relapsed 2 or more years after diagnosis and didn’t have a combined relapse (bone/lung)7. Patients recurring with non-lung distant metastases only or any combination of local relapse, lung metastases and non-lung metastases had comparatively worse overall survival8.
Central nervous system (CNS) metastases in osteosarcoma at presentation or at relapse are very rare and have been reported only in a few cases. The mode of CNS metastasis in osteosarcoma is usually hematogenous and is commonly associated with pulmonary metastases9. The postulated mechanism is the migration of tumour emboli from the lung to the brain. Clinical presentation may include seizures, status epilepticus, hemiparesis, raised intracranial tension or stroke-like presentation. Most published reports on CNS involvement in osteosarcoma describe presentations occurring in the primary disease setting, with fewer studies detailing CNS metastases arising during disease progression or relapse. The majority of them have supratentorial CNS involvement. The cerebellar lesion reported by Niaz et al. in a 16-year-old boy is an extremely rare presentation. A distal femur lesion was confirmed as the primary lesion later on workup. The clinical course was rapidly progressive, requiring urgent posterior fossa decompression; however, the child did not survive the postoperative period10. Like in our case, most of the reported cases have solitary metastasis. Multiple metastases involving the frontal lobe have been described in a 22-year-old woman who had a stroke-like presentation. The primary lesion in this case was the right iliac bone, an axial site11. Both of these cases had pulmonary metastasis too, supporting the hypothesis of tumour emboli migration from the lung. An alternate mode of spread, bypassing the lung, has been reported by Menassa et al. in a 12-year-old boy with osteosarcoma of the fibula and frontoparietal cortical lesions. The patient had a patent foramen ovale, which probably allowed neoplastic cells to reach the brain without being filtered through the lungs12. An increased risk of brain metastasis with metastatic disease at presentation or with recurrence at 1 year has been reported in osteosarcoma13. Yonemoto et al. recommend regular brain imaging in patients with active pulmonary metastases14. Marina et al. had a similar consensus in those with metastatic disease at diagnosis or those who have recurrence within 12 months15. The key findings from the literature review are summarised in Table 1.
Table 1: Baseline characteristics, treatment, and outcome of patients with brain metastasis
| Menassa et al. (1997) | Niazi et al. (2009) | Dwivedi et al. (2011) | Marina et al. (1993) | |
|---|---|---|---|---|
| Type of report | Case report | Case report | Case report | A series of 13 patients |
| Demographics | 12 years/Male | 16 years/Male | 22 years/Female | Ages 4–25 years |
| Clinical features | Headache, raised ICP | LOC* Cerebellar hemorrhage | Right hemiparesis, LOC* | Headache, seizures, focal deficits |
| CNS lesion characteristics | Multiple hemorrhagic supratentorial lesions | Hemorrhagic posterior fossa mass | Multiple frontal hematomas | Varied; supratentorial, cerebellar, etc. |
| Primary tumour site | Left fibula | Right distal femur | Right iliac bone | Mostly long bones |
| Lung metastases | None | Present | Present | Present in 12/13 |
| Treatment | Biopsy + resection | Posterior fossa decompression | Supportive/emergent | Response to Ifosfamide |
| Outcome | Not stated | Died | Poor prognosis implied | 1 long-term survivor; others died |
Given the rarity of the disease, there are no guidelines regarding optimal management of brain metastases of osteosarcoma. Effective intracranial control remains difficult as brain metastases from sarcomas are highly radio- and chemo-resistant, and surgical resection is the basic treatment. The achievement of a second complete resection of the disease has been associated with a better long-term survival after recurrence16. Our patient had progression of the primary lesion along with intracerebral recurrence, which portends a very poor outcome, and unfortunately succumbed to the disease. Given the clinical and radiological evidence in this setting, an alternate diagnosis seems very unlikely. However, the absence of histopathological confirmation is definitely a shortcoming in our case.
Conclusion
Brain metastases are extremely unusual in osteosarcoma patients, and clinicians should be aware of this possibility when an osteosarcoma patient presents with neurological symptoms. Currently, there is no consensus on the optimal management of such patients, and their prognosis is poor.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
License
© Author(s) 2025.
This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, and unrestricted adaptation and reuse, including for commercial purposes, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
References
-
Youn P, Milano MT, Constine LS, Travis LB. Long-term cause-specific mortality in survivors of adolescent and young adult bone and soft tissue sarcoma: a population-based study of 28,844 patients. Cancer. 2014 Aug 1;120(15):2334-42.
-
Meyers PA, Heller G, Healey JH, Huvos A, Applewhite A, Sun M, LaQuaglia M. Osteogenic sarcoma with clinically detectable metastasis at initial presentation. J Clin Oncol. 1993 Mar;11(3):449-53.
-
Kempf-Bielack B, Bielack SS, Jürgens H, et al. Osteosarcoma relapse after combined modality therapy: an analysis of unselected patients in the Cooperative Osteosarcoma Study Group (COSS). J Clin Oncol. 2005 Jan 20;23(3):559-68.
-
Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002 Feb 1;20(3):776-90.
-
Hazewinkel AD, Lancia C, Anninga J, van de Sande M, Whelan J, Gelderblom H, Fiocco M. Disease progression in osteosarcoma: a multistate model for the EURAMOS-1 (European and American Osteosarcoma Study) randomised clinical trial. BMJ Open. 2022 Mar 4;12(3):e053083.
-
Marina NM, Smeland S, Bielack SS, et al. Comparison of MAPIE versus MAP in patients with a poor response to preoperative chemotherapy for newly diagnosed high-grade osteosarcoma (EURAMOS-1): an open-label, international, randomised controlled trial. Lancet Oncol. 2016 Oct;17(10):1396-1408.
-
Spraker-Perlman HL, Barkauskas DA, Krailo MD, et al. Factors influencing survival after recurrence in osteosarcoma: A report from the Children’s Oncology Group. Pediatr Blood Cancer. 2019 Jan;66(1): e27444.
-
Gelderblom H, Jinks RC, Sydes M, et al. European Osteosarcoma Intergroup. Survival after recurrent osteosarcoma: data from 3 European Osteosarcoma Intergroup (EOI) randomised controlled trials. Eur J Cancer. 2011 Apr; 47(6):895-902
-
Nieto-Coronel MT, López-Vásquez AD, Marroquín-Flores D, Ruiz-Cruz S, Martínez-Tláhuel JL, De la Garza-Salazar J. Central nervous system metastasis from osteosarcoma: Case report and literature review. Rep Pract Oncol Radiother. 2018 Jul-Aug;23(4):266-269.
-
Niazi TN, Forester C, Afify Z, Riva-Cambrin J. Osteosarcoma presenting as hemorrhagic cerebellar metastasis. Childs Nerv Syst. 2009 Dec;25(12):1643-7.
-
Dwivedi AN, Gupta PK, Gupta K, Garg G. Hemorrhagic brain metastasis from osteogenic sarcoma of iliac bone in young female: unusual site of presentation. Neurol India. 2011 Jul-Aug;59(4):639-40.
-
Menassa L, Haddad S, Aoun N, Slaba S, Atallah N. Isolated brain metastases of osteosarcoma in a patient presenting with a patent foramen ovale. Eur Radiol. 1997;7(3):365-7.
-
Kebudi R, Ayan I, Görgün O, Ağaoğlu FY, Vural S, Darendeliler E. Brain metastasis in pediatric extracranial solid tumors: survey and literature review. J Neurooncol. 2005 Jan;71(1):43-8.
-
Yonemoto T, Tatezaki S, Ishii T, Osato K, Takenouchi T. Longterm survival after surgical removal of solitary brain metastasis from osteosarcoma. Int J Clin Oncol. 2003 Oct;8(5):340-2.
-
Marina NM, Pratt CB, Shema SJ, Brooks T, Rao B, Meyer WH. Brain metastases in osteosarcoma. Report of a long-term survivor and review of the St. Jude Children’s Research Hospital experience. Cancer. 1993 Jun 1;71(11):3656-60.
-
Shweikeh F, Bukavina L, Saeed K, Sarkis R, Suneja A, Sweiss F, Drazin D. Brain metastasis in bone and soft tissue cancers: a review of incidence, interventions, and outcomes. Sarcoma. 2014;2014:475175.





